
Dear colleagues, September 28 2014 Eindhoven, the Netherlands
Let me first introduce myself , because you may not all know me.
I am a cardiothoracic surgeon at Catharina Hospital , Eindhoven , the Netherlands.
Mostly doing all cardiothoracic procedures , except congenital cardiac procedures.
Having learned from my teachers, how to do the classical surgical correction for thoracic wall deformities, I have added these operations to my specialties . My technique for pectus excavatum is a mixture of Daniel ( Nashville , Tennessee 1958) and Sanger , Tayler and Robicsek (1963) .
And with these operation my patients were satisfied.
Some 5 years ago , a girl of 15 years of age came with her mother to my outpatient clinic and ask for a Nuss bar , because her cousin had such an operation with good results.
I told her that i never did or even saw a Nuss bar , but that this technique looked to me an attractive alternative to my own one.
Promising her and her mother to we delved into this technique we went to a chest wall meeting in Ismir 2009 , where we met Dr Pilegaard.
After visiting him in Denmark he helped us with our first 2 cases, and from there we went on.
Because my fellow cardiac surgeons asked me what the fate was of the mammary arteries I did a study about this matter which was recently published : Patency of the internal mammary arteries after removal of the Nuss bar: an initial report ( pub Interactive cardiovasc Thoracic Surgery , 2014 , Vol 19(1) pp 6-9 . Now we can visualize the mammary arteries with MRI .
Having done only 150 Nuss bar procedures I am a rookie in the group .So far my results are excellent , having only few complications , in line of the current era. Knowing that age limits for the Nuss Bar procedure is shifting forward I started operating on adults as well.
I would ask the group now for some advice here is my case:
58 year old female with symptoms that fitted with pectus excavatum in adult age; physical condition less,etc.
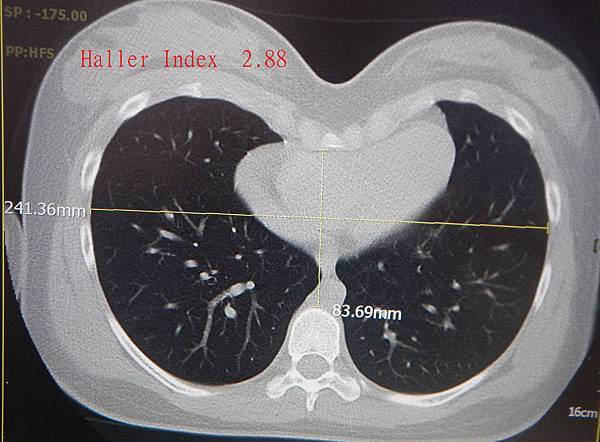
Haller index was 6.5 . see picture 1-3 for preoperative imaging.
On the 8 th of October 2013 I put in two Nuss bars , 12 and 11 inch with lateral side bars only on the left.
The where wider than I usually use, but I felt this was a more solid construction in this particular case.
The procedure itself was very easy and quick , like I was operating a 18 year old girl.
Being proud that also could do Nuss bars in patients over 50 years of age , the first disappointment came soon : lot of pain , despite epidural post op and a lot of pain killers.
Post operative x-rays are shown in picture 4 and 5.
On May 2014 I saw her , just before she went on a holiday to Portugal.
There the situation got really worse: she had fever, elevated CRP , x-rays are shown in picture 6.
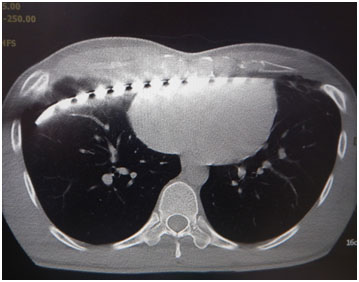
Diagnosed as pneumonia , treated with antibiotics I saw her back in the Netherlands ( ct scan and x-rays are in figure 9).It is always helpful to provide your patients with the last x-rays of the bar in place , so that where ever they might travel to , local physicians can compare the position of the bar , that is what I always do. The all have cellphone so I mail the pictures to them. Bars Did not looked displaced neither on x-rays or ct scan.
Because she had so much pain , and my suspicion that the lower bar at the right side might have caused pleural irritation , we finally decided to remove the lower bar. This gave some release of the pain.
When removing the lower bar I saw that the bar did not enter the thoracic cavity but only pushed 5 rib ( which you can see on the ct scan , picture 10 d)
What was the cause of her fever , elevated CRP and pain??
Was it allergy? Or bad surgery? I know from an article from the clinic of Nuss ( When it is not an infection : metal allergy after the Nuss procedure repair of pectus excavatum. J ped surg 2007 Jan ;4291) 93-7 that allergy is possible.
There might be other causes for these symptoms.
She will visit me soon , and has ask me to consider the possibility to remove the other bar and to convert to a classical procedure.
She still trust me , but ask me to discuss this matter with some experts, which is done by this email.
Questions:
Was the initial procedure good?
What was the cause of the fever and pain and elevated CRP in Portugal.
Was it the right decision to remove the lower bar.
Might this be a case of allergy to nickel?
What to do now?
Testing for Ni allergy?
If positive , is removing the upper bar and placing 2 new titanium ones an option.
Convert to classical operation?
Is a partial incision in the sternum like described by Ravenni , 2013 an option to have less forces and pain ?
Yours sincerely, Ted Elenbaas , CWIG , member
Cardiothoracic Surgeon , Catharina Hospital Eindhoven, the Netherlands

 H
H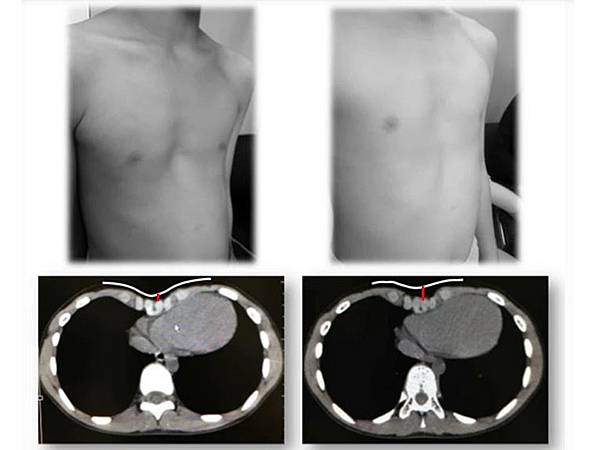







 {{ article.title }}
{{ article.title }}